Do you have keratoconus? Keratoconus is a serious eye condition that can affect your sight and vision progressively over time.
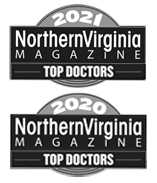
Keratoconus occurs when the cornea gradually becomes thinner over time. When the cornea gets thinner, it also becomes more cone-shaped, leading to distorted vision, sensitivity to light, and blurry vision.
Many eye doctors begin treating keratoconus with special contact lenses that help to correct corneal distortion. As it progresses, you may need to consider another treatment known as corneal cross-linking.
Leaving keratoconus untreated makes it harder and harder to see over time. Undergoing corneal cross-linking if you have keratoconus helps to slow or halt the progression of the condition.
The treatment is minimally invasive and doesn’t require the use of surgical techniques. If you have keratoconus, especially in the early stages, you may see a significant benefit from corneal cross-linking.
But how do you know if you have keratoconus and what treatment is best for you? Keep reading to learn everything you need to know when it comes to keratoconus and corneal cross-linking!
What is Keratoconus?
Keratoconus is a condition that occurs when the cornea thins out and becomes a cone-like shape, causing vision problems. The cornea is the front part of your eye that light passes through, and when you change the way light moves through, it can distort your vision.
For example, nearsightedness and farsightedness are caused by having a cornea that is slightly convex or slightly concave in shape. While you can correct these refractive errors with glasses or contacts, keratoconus is a more concerning condition.
Your cornea isn’t meant to become thinner, and when it does, it’s more likely to become inflamed and develop scar tissue. If any scar tissue does start building up on the cornea, this can make your vision even worse.
All the while, having a misshapen cornea that’s cone-shaped instead of dome-shaped leads to distorted vision. Over time, this can make it impossible to wear contact lenses.
Keratoconus typically starts appearing in people who are in their late teens or early twenties. After this, it may continue progressing for 10-20 years before it slows down or stabilizes.
Who is at Risk for Keratoconus?
Anyone is at risk for developing keratoconus, including both men and women. The exact cause of keratoconus has yet to be determined. This makes it more challenging to assess whether you may be at risk for developing the condition.

However, there are a few factors some patients have in common. These include:
- Having a family history of keratoconus
- Connective tissue disorders like Marfan or Ehlers-Danlos syndromes
- Allergic conjunctivitis
- Excessive eye rubbing that’s often a result of allergy symptoms
The best way to mitigate your risk for keratoconus is to avoid rubbing your eyes. Rubbing your eyes is something you should avoid doing whenever possible, as it can lead to eye infections and other eye-related issues.
Otherwise, if you have one of these risk factors, you should be aware of your risk and see your eye doctor regularly. You should also know the primary symptoms of keratoconus.
What are the Symptoms of Keratoconus?

Keratoconus presents a few symptoms even in the early stages of the condition. These include:
- Distorted vision
- Blurry vision
- Irritation and swelling
- Light sensitivity
As the disease progresses and the cornea becomes thinner and weaker, it can lead to other symptoms, like increased nearsightedness and an inability to wear contacts. It’s best to have keratoconus diagnosed early to avoid these late-stage symptoms and have the best treatment prognosis.
If you have symptoms, see your eye doctor immediately to ensure early diagnosis and treatment.
What is Corneal Cross-Linking?
Corneal cross-linking is a treatment for progressive keratoconus. It cannot reverse the disease, but it can slow it or stop it from progressing further and preserve your remaining vision.
Having corneal cross-linking may allow patients to avoid having a corneal transplant later on. Other treatment methods for keratoconus involve surgery to correct the shape of the eye, but they can’t stop the condition from getting worse and progressing. Corneal cross-linking is non-invasive, making it not only effective but also more convenient for patients.
How Does Corneal Cross-Linking Work?
Corneal cross-linking aims to strengthen your corneal tissue so it doesn’t become any thinner. This is possible with a combination of prescription eye drops and UV light.
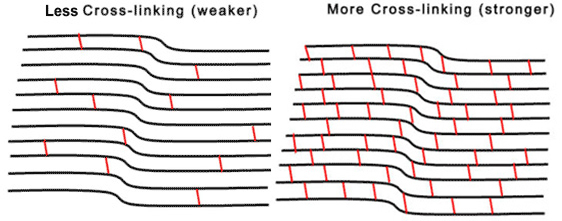
By using prescription eye drops and UV light, new collagen cross-links are created. Collagen cross-links are the bonds between the collagen fibers that make up the cornea. Strengthening these cross-links helps the cornea become stiffer, which also supports it.
The procedure involves first having your eyes numbed with topical anesthetic drops. After numbing your eyes, your eye doctor will remove the epithelium. The epithelium is the thin layer on the cornea’s surface.
Removing the epithelium is necessary because it helps the topical anesthesia drops penetrate the cornea’s tissue. Once the epithelium has been entirely removed, your cornea will be able to absorb the UV light, and the riboflavin eye drops more effectively.
Once the eye drops take effect, you’ll sit back and stare at a light aimed directly at your eye. The whole procedure is painless and often doesn’t take more than an hour, but the results can be vision-saving.
You will be at your eye doctor’s office for about two hours to allow plenty of time for recovery before you can return home. Stronger, shorter bonds between collagen fibers in your cornea mean a stronger cornea, which can stop progressive keratoconus and prevent further symptoms.
Is Corneal Cross-Linking Right for You?
Corneal cross-linking is best for patients with early to progressive keratoconus. You can undergo corneal cross-linking at different points, but it’s most effective for patients at the early stages.
Corneal cross-linking cannot reverse keratoconus, so if your vision has already become severely distorted, you may require a surgical procedure as well as corneal cross-linking.
Early diagnosis and treatment are vital when it comes to keratoconus, which means you should be vigilant when it comes to your eye health. Make sure you see an eye doctor for regular exams, especially if you’re an at-risk group so that you can get an early diagnosis and treatment.
Are you wondering if you may be a candidate for corneal cross-linking? Schedule an appointment at See Clearly Vision with one of our eye doctors in Tysons Corner or Arlington to discuss your options today!